Pharmacological induction
Induction of labor is the administration of drugs and the use of obstetric maneuvers in order to begin labor.
Induction may be indicated in some situations, for example:
- maternal pathology
- fetal pathology
- no onset of labor within 12-24 hours after rupture of the membranes (breaking water);
- chronologically prolonged gestation: gestation of more than 41-42 weeks.
The drugs used in an induction depend on the condition of the woman's cervix (degree of softening, shortening and dilation) and the degree of attachment of the fetal head.
Depending on the condition of the cervix and fetal head, it may be done with prostaglandins or directly with amniorexis and oxytocin.
'Pharmacological induction', d'Virtual Nurse, content under license CC BY-NC-ND 3.0 ES, with modifications made by the Gynecology and Obstetrics Service of the Hospital de Sabadell
Oxytotic stimulation
Birth stimulation is about administering oxytocin to the pregnant woman, usually intravenously, with the aim of provoking contractions or of increasing their intensity and frequency in order to accelerate labor, in the case that it is in a latent phase.
'Oxytotic stimulation', d'Virtual Nurse, content under license CC BY-NC-ND 3.0 ES
Non-pharmacological induction
Non-pharmacological induction methods have traditionally been used.
- Sex. They cause the woman to secrete oxytocin and the man, seminal prostaglandins, which can help soften the cervix and lead to delivery.
- The complementary therapies. They offer alternatives to help start labor, such as nipple stimulation, which results in oxytocin secretion, acupuncture, shiatsu, etc.
'Non-pharmacological induction', d'Virtual Nurse, content under license CC BY-NC-ND 3.0 ES, with modifications made by the Gynecology and Obstetrics Service of the Hospital de Sabadell
Amnioscopy
It is a technique used to see the color of the waters, when the membranes have not yet broken, using an apparatus called an amnioscope and a lamp. It is a procedure that is rarely used due to the existence of other methods of fetal control.
'Amnioscopy', d'Virtual Nurse, content under license CC BY-NC-ND 3.0 ES, with modifications made by the Gynecology and Obstetrics Service of the Hospital de Sabadell
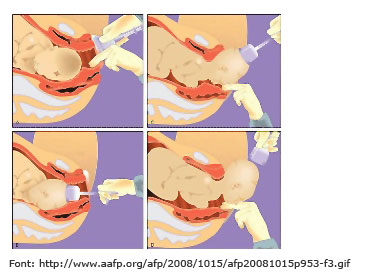
Amniotomy
Amniotomy is indicated in the induction of labor, in the passage of birth, and when there is a suspicion of a loss of fetal well-being after assessing the color and amount of water.
'Amniotomy', d'Virtual Nurse, content under license CC BY-NC-ND 3.0 ES, with modifications made by the Gynecology and Obstetrics Service of the Hospital de Sabadell
Episiotomy
It is an incision made in the vagina to expand the space and thus accelerate fetal outflow. It affects the skin, muscle and vaginal mucosa and requires suture once the fetus and placenta have left.
The episiotomy is performed with scissors during the expulsion phase, at which point the cephalic presentation of the crown occurs, that is, when the fetal head exits and presses the perineum. This is usually done under regional or local anesthesia. The WHO questions its indiscriminate use and recommends restricted practice, considering each case individually.
Episiotomy is indicated when the birth attendant thinks it is necessary, usually in the following cases:
- Small distance between vagina and anus. There is an average distance of 3,9 cm between the anus and the vagina; if the distance is less than 2,5 cm, the risk of perineal injury is increased by 10 times.
- Rigid perineal muscle. This is due to the lack of elasticity of the perineum.
- Mutilation scars of female genitalia or third and fourth degree tears in previous parts. They make it difficult to relax the muscles.
- Loss of fetal well-being. It makes it necessary to shorten the expulsion period so that the fetus is born as soon as possible.
- Part complicated. It requires the use of instruments such as forceps or spatulas.
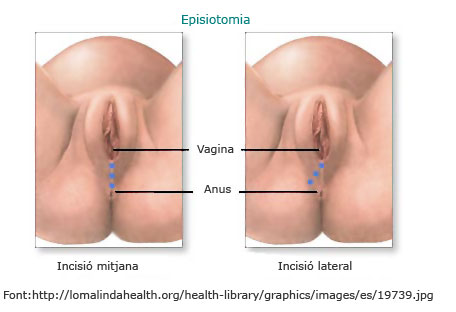
El perineal massage prenatal during the last weeks of gestation is effective in preventing perineal trauma and episiotomies, especially in women expecting a first child or having undergone an episiotomy.
'Episiotomy', d'Virtual Nurse, content under license CC BY-NC-ND 3.0 ES, with modifications made by the Gynecology and Obstetrics Service of the Hospital de Sabadell
Obstetric instrumentation
These are the use of forceps, Thierry's spatulas or the vacuoextractor or obstetric suction cup to shorten labor and speed up birth. Instrumentation may be needed in the following situations:
Maternal indications
- Maternal exhaustion. Long births can exhaust the mother to the point of hindering the expulsion phase, in which the pregnant woman has to push firmly and steadily to help the baby be born. In this situation, the uterine muscle may also be depleted, which in very long parts reduces the effectiveness of contractions.
- Excessive analgesia. If theperidural anesthesia it has been given in excessive doses or the woman is very sensitive to this type of drug, the pregnant woman can reach the expulsion stage without any sensations. If the woman does not feel the pressure of the contraction and of the fetal head, nor the power, she can hardly give birth without help.
- Prolonged expulsion. It occurs in cases where the evolution of fetal output is stopped. The duration of the expulsion period it depends on whether you use peridural anesthesia or whether it is the first birth. Generally, deliveries with peridural anesthesia of a first child usually have an expulsion phase that can reach four hours; however, with the second child and without peridural anesthesia, the time taken from the full dilatation to the exit of the fetus is considered to be one hour.
- Maternal illness. Some diseases, such as heart disease, a maternal infection, etc., make it advisable to shorten the expulsion period.
Fetal indications
- Loss of fetal well-being. It makes it necessary to accelerate the birth.
- Rotation dystocia. The fetus is not properly positioned in the maternal pelvis.
Obstetric instrumentation can be done with the instruments described below:
- Forceps
The forceps are metal claws, fenestrated, formed by two branches that connect to each other. These branches are inserted apart into the vagina and placed one on each side of the fetal head; then they articulate and the fetal head is rotated, on which traction is exerted until it exits. It is a contraindicated instrument in premature, due to the pressure exerted on the head. To practice this technique, anesthesia should be applied, the water pouch must be broken, the dilation should be complete and the fetal head should be located in the lower strait of the pelvis.
Complications:
- injuries to the maternal tissues: cervix, vagina and muscle;
- marks or small temporary wounds on the fetal head;
- craniofacial injuries or fractures in the fetus.
 Source: Lucia Alcaraz and Julia Cid
Source: Lucia Alcaraz and Julia Cid
- Thierry spatulas
Thierry spatulas or spatulas are two metal spoons that act as a shoe or slide for the fetal head. Unlike forceps, these spoons do not hinge or push, but instead expand the vaginal space to help the fetus descend and exit. The criteria for application and the complications are similar to those for the use of forceps, although there is an increased risk of injury to the maternal tissues.
 Source: Lucia Alcaraz and Julia Cid
Source: Lucia Alcaraz and Julia Cid
- Vacuum extractor or suction cup
This is a cup or bell that is placed over the fetal head, in which a negative pressure is applied until the vacuum is reached. The vacuum causes the cup to attach to the head of the fetus and to allow for traction, intermittently and synchronously with the uterine contraction. It takes about 10 to 20 minutes to reach the progressive vacuum, so this instrument is not used in case of acute fetal suffering, which requires rapid removal. The suction cup can be applied without anesthesia.
The vacuoextractor is indicated in situations similar to those that apply forceps and spatulas, but with the limitation of time; therefore it is not recommended in emergency situations. Nor can it be used in premature because of the negative pressure it exerts on the head, as it increases the risk of the baby having an intracranial hemorrhage.
The suction cup has less maternal complications than the forceps or the spatulas. Fetal complications include: lesions in the area to which the cup is attached, cephalohematoma (accumulation of blood under the scalp that spontaneously resorbs in a few days), and intracranial hemorrhage.
'Obstetric instrumentation', d'Virtual Nurse, content under license CC BY-NC-ND 3.0 ES, with modifications made by the Gynecology and Obstetrics Service of the Hospital de Sabadell
Cesarean section
Cesarean section is a surgical operation that aims at the birth of the fetus and the removal of the membranes and placenta through the abdominal cavity. The approach to the fetus is usually through a suprapubic transverse incision, called the Pfannenstiel incision. The skin can be sutured with staples or nylon thread, which must be removed seven to ten days after surgery; the internal sutures resorb over time.
The intervention takes approximately 30 to 60 minutes and is usually performed under regional anesthesia (epidural or spinal cord), with the advantage that the mother is fully aware and can see the newborn immediately. General anesthesia is rarely needed.
There are two types of caesarean section. Elective cesarean section is one that is scheduled before the birth starts for different indications. Resuscitation cesarean section is one that is indicated during the course of labor.
Complications
Medical advances have made cesarean sections more secure, but maternal and fetal morbidity rates by cesarean section are still important when compared to those for vaginal delivery.
'Cesarean section', d'Virtual Nurse, content under license CC BY-NC-ND 3.0 ES, with modifications made by the Gynecology and Obstetrics Service of the Hospital de Sabadell
Other interventions
Apart from the obstetrics, there are a number of general interventions that take place in the delivery rooms.
- Placement of an intravenous route. An intravenous route to the woman is placed in our delivery room.
- Bladder catheterization. Occasional non-permanent urinary bladder catheterization is recommended for women undergoing peridural anesthesia, as a full bladder can be an obstacle for the baby to come out. Permanent bladder catheterization is indicated for women who need a caesarean section.
- Enema. Traditionally, an enema was administered to all women entering a delivery room with the aim of cleaning the rectum to reduce the risk of infection. This practice is completely outdated, painful and uncomfortable for the woman, does not guarantee that the rectum is free of stool at birth, nor does it reduce the risk of perineal infection. Generally, the woman evacuates several times during the prodromal and dilatation phase spontaneously. Administration of enema it should be limited to those women who request it expressly or those who have a full rectal ampoule and cannot evacuate spontaneously.
- Shaved. Shaving of the pubic and genital area has also been widespread practice in delivery rooms. The purpose of the shaving was to empty the genital area of hair in order to increase labor asepsis and to facilitate the work for the assistant who had to suture the tear or episiotomy. Like the administration of enemas, it is an obsolete and painful practice for the woman. The shaving should then be avoided and replaced with a scalp cut, limited to the area to be sutured. In the case of a caesarean section, it is recommended to shave only the highest part of the pubic hair and immediately before the operation.
- I leave. Since Mendelson's Syndrome (which is the passage of gastric contents into the lungs) was described in 1946, fasting before birth was recommended. It should be remembered, however, that this syndrome occurs only when the person is below general anesthesia or when unconscious. Since 1970 regional anesthesia has displaced the general in all fields of surgery, in particular the field of obstetrics; therefore, the risk of developing this syndrome has decreased.
Therefore, fasting during childbirth is a disused practice, which can lead to complications:
- It does not guarantee that the stomach is empty (the digestions of the pregnant women are slower).
- Increases the acidity of the gastric contents as it increases the production of hydrochloric acid; the severity of Mendelson's syndrome is related to the volume of the aspirated contents and the acidity.
- It can cause dehydration.
- It can cause hypoglycemia (lowering blood glucose) and lead to ketosis (imbalance in metabolism which indicates that the stored fat reserves in the body are being consumed); these situations involve:
- nausea and vomiting,
- headache,
- sweats, visual disturbances and loss of consciousness,
- maternal exhaustion;
- slowing labor, due to a decrease in the frequency and strength of contractions, and an increased risk of complications (which can lead to instrumental birth);
- commitment in contributing energy to the fetus and loss of fetal and neonatal well-being.
- Hydration during labor: A woman who does not have risk factors needs to drink fluids during labor and should be encouraged whether she wants epidural anesthesia or not. It is recommended to bring isotonic water or drinks for consumption for labor
'Other interventions', d'Virtual Nurse, content under license CC BY-NC-ND 3.0 ES, with modifications made by the Gynecology and Obstetrics Service of the Hospital de Sabadell