- Edu Soler
- no comments
Most aspects of medicine have historically been learned in an apprenticeship model by means of observation, imitation, and instruction. This paradigm is rapidly changing towards the adoption of medical simulation. This is due to the irruption of more technology in surgeries and due to law maturation in the field. The following report captures the most interesting data of the field.
Commonly regarded essential competencies include manual dexterity, familiarity with high-tech equipment, sound professional judgment, and the ability to integrate technical skills with clinical practices. However, the incongruity between evidence-based recommendations and real-world practice highlights the inadequacy of the preceptored medical education tradition. Consequently, there has been a shift in the method of medical education towards experiential (‘hands-on’) medical learning (1).
Surgical simulation enhances surgical skills by allowing repeated practice and to maintain an acquired level of competence. Current high fidelity simulators offer the opportunity for safe, repeated practice and objective measurement of performance. Furthermore, it is a more efficient and cost-effective modality that poses no risk to patients and avoids many ethical and legal complications.
Although some form of simulation has existed for decades in surgical training, we are truly in the infancy stages of incorporating simulation into residency education. Beginning in July 2008, the Accreditation Council for Graduate Medical Education (ACGME) Residency Review Committee for Surgery mandated that all surgery residency programs incorporate simulation within the curriculum of their program. Even surgical simulation adoption is highly increasing in hospitals, many discussions remain open about if competencies acquired in the sim lab translates to clinical competence (2).
Also, Virtual Reality (VR), or Virtual Environments (VE), -based simulators are rapidly becoming an integral part of surgical training and skills assessment.
Over the last twenty-five years, there has been a strong movement towards changing the traditional approaches to surgical training. One of the major drivers for the development of surgical simulation is the advent of new surgical practices such as interventional radiology and MIS techniques. Example: bronchoscopy and laparoscopy.
| Surgical Simulation | Ultrasound Simulation |
| Laparoscopic Surgical Simulators | Anesthesia |
| Arthroscopic Surgical Simulators | Cardiology |
| Cardiovascular Simulators | Emergency Medicine |
| Obstetrics and Gynecology Simulators | Intensive Care Unit |
| Orthopedic Simulators | OB/GYN |
| Spine Simulators | Radiology |
| Endovascular Simulators | Others (Urology, General Nursing, Pediatrics) |
The complexity of instrument controls, restricted vision and mobility, difficult hand-eye coordination, unnatural perceptual-motor relationships, and the lack of tactile perception requires a high degree of manual dexterity and coordination from the operator. Consequently, much attention has been directed to new training methods such as surgical simulators for acquiring these skills (4).

Operating theater apprenticeship
Conventional surgical training is based on the apprenticeship model. Under the scrutiny of experienced instructors, surgical trainees learn by observing, then gradually performing specific procedures inside the operating theatre. Although the operating theatre is a basic element of surgical training, it is becoming less effective due to several factors. First, trainees are exposed to the heterogeneous distribution of procedures depending on the flow of patients; it is also time-consuming and costly. Moreover, operating theatre-based training can constitute a potential risk to patients due to the inevitable distraction while training on complex or advanced procedures. (1)

Animals and Cadavers
Students traditionally learn the basics of surgery on live lab animals. For example, the use of surgical instruments begins with anatomical dissections and physiological experiments. Anesthetised animals, typically pigs or rats, have long been a part of the curriculum in medical schools. However, this training modality is becoming increasingly unacceptable due to obvious ethical, legal, and human concerns. It is not only because of the tendency towards avoiding animal sacrifices for teaching purposes, but also because some infectious diseases can be transmitted from animals to trainees. Moreover, from a technical point of view, the anatomy of animals and human beings are different, and the cost associated with preserving and disposing of used models is high (1).
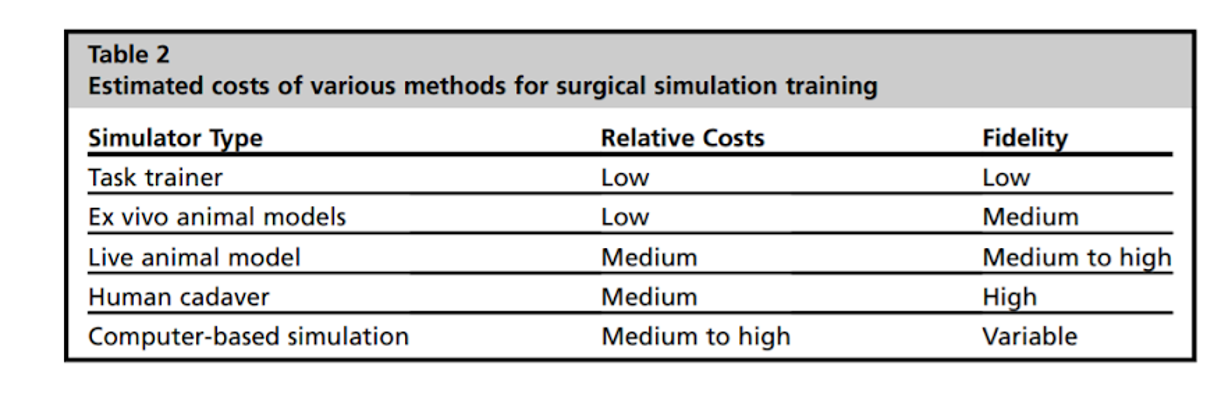
The most realistic, high-fidelity model remains human cadaver. Cadaver costs fall into a modest price range, relative to other high-fidelity synthetic models (2).

Synthetic Models - task trainers
Synthetic models provide a low-risk training opportunity. Many models resembling parts of the human anatomy with complexity ranging from bone structures to fully integrated models are available. In practice, training with synthetic models is usually used during the preliminary stages of surgical education. This modality, however, has limited realism and it is also difficult and costly to acquire and maintain a large number of different cases (1).
When considering the cost of simulation, task trainers may provide an economically viable alternative to high-fidelity and high-cost models. There are some examples in the literature showing the viability of simulation models for acquiring performing skills. As an example, Helder and collaborators demonstrated to improve aortic anastomosis in medical students and residents by using a low-cost aotic anastomosis model ($22.50/unit), with pretest and posttest skills performed on a high-fidelity model (6).

Computer Based training
One of the established training methods is based on interactive multimedia applications where the trainee interacts visually with the system in order to learn the necessary steps involved in certain surgical procedures. Nevertheless, it is still inadequate for providing effective training on basic surgical skills. This is largely due to the difficulty of imitating surgical procedures by using the Two-Dimensional (2D) CBT systems that have limited immersion, physical control, and interaction (1).
Additive manufacturing and 3D scanning are contributing significantly to the advancement of computer-based training. Specifically, in surgical simulation are becoming a key technology for surgery planning and improving surgical outcomes. Also, Virtual Reality and Augmented Reality are emerging technologies in healthcare education and, although there are still limited randomized studies comparing its impact with the standard methods, some authors already suggest the importance of this technologies in improving quality of patients’ care.
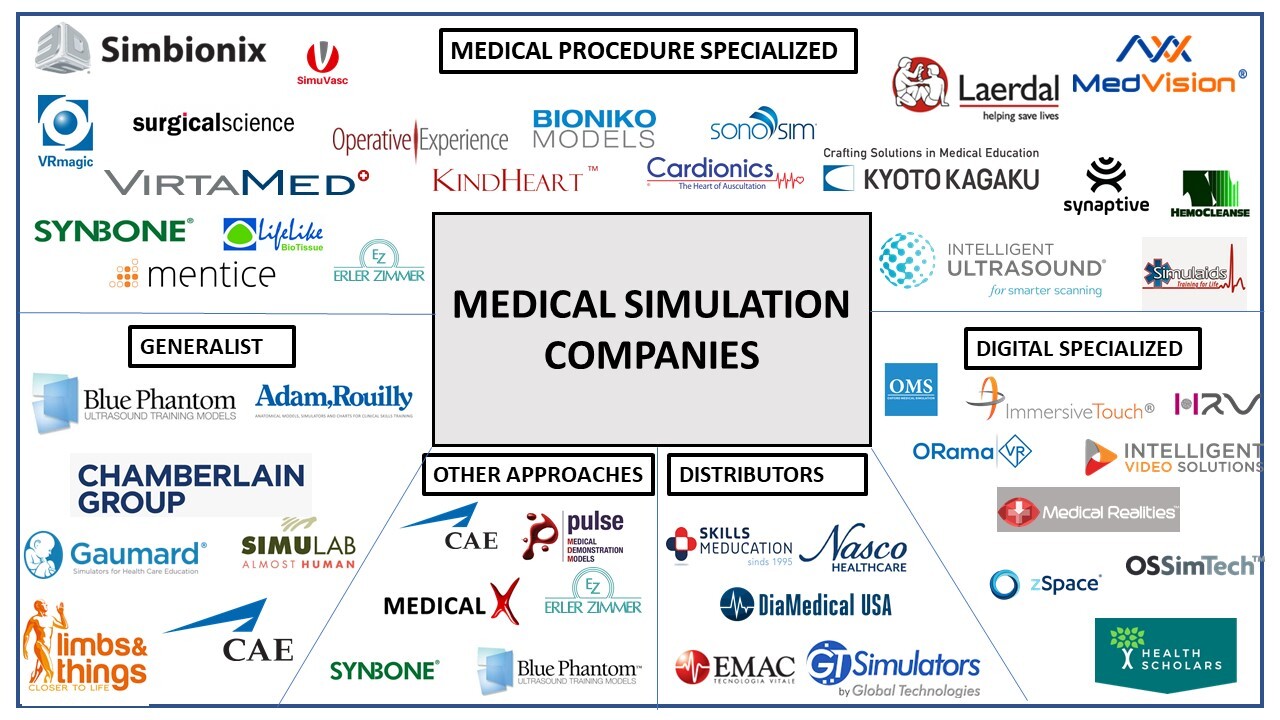
In this analysis, it has been determined the different types of medical simulation companies. Medical training market has demonstrated to be big enough to consolidate big, medium, and small corporations, also distributors, and very specialized companies. The market can be classified according to the following paramaters:
- Medical procedure specialized companies: These ones are producing products for small amounts of clinical areas. For example, SimuVasc is just specialized in vascular procedures or Synbone is specialized in the production of bone models.
- Generalists: These ones are producing products for all the clinical areas. They offer large portfolios of products with less focus on the specialization.
- Other approaches: These ones are producing products out of medical training or other approaches. For example, Medical X is specialized in military medical training, or Laerdal is specialized in experiential training.
- Distributors: These ones are not producing simulators, they have licencing deals with producers to sell their products.
- Digital specialized: These ones are incorporating digital technology instead of simulators. For example, Oxford Medical Simulations are specialized in VR or Intelligent Video Solutions are specialized in video platforms.
The scientific societies have a critical role in the application of medical simulation in healthcare. They serve as a resource for young professionals in their growth in medical education and administration. Here you can check the most relevant societies worldwide:
| Logo | Name | Website |
 |
Society in Europe for Simulation Applied to Medicine (SESAM) | link |
 |
Federación Latinoamericana de Simulación Clínica y Seguridad del Paciente (FLASIC) | link |
 |
Canadian Network for Simulation in Healthcare (CNSH) | link |
 |
Harvard Center for Medical Simulation | link |
 |
Society of Simulation and Health Care | link |
 |
Scandinavian Simulation Society | link |
 |
Sociedad Española de Simulación Clínica y Seguridad del Paciente (SESSEP) | link |
| Editorial | Journal | SCIMAGO h-index | Website |
 |
SAGE – Simulation / Simulation and Gaming | 48 / 57 | link |
 |
Journal of the Society for Simulation in Healthcare | 46 | link |
 |
Clinical Simulation in Nursing | 36 | link |
 |
BMJ’s Simulation & Technology Enhanced Learning | 7 | link |
 |
Advances in Simulation – BMC part of Springer Nature | – | link |
MARKET SIZE
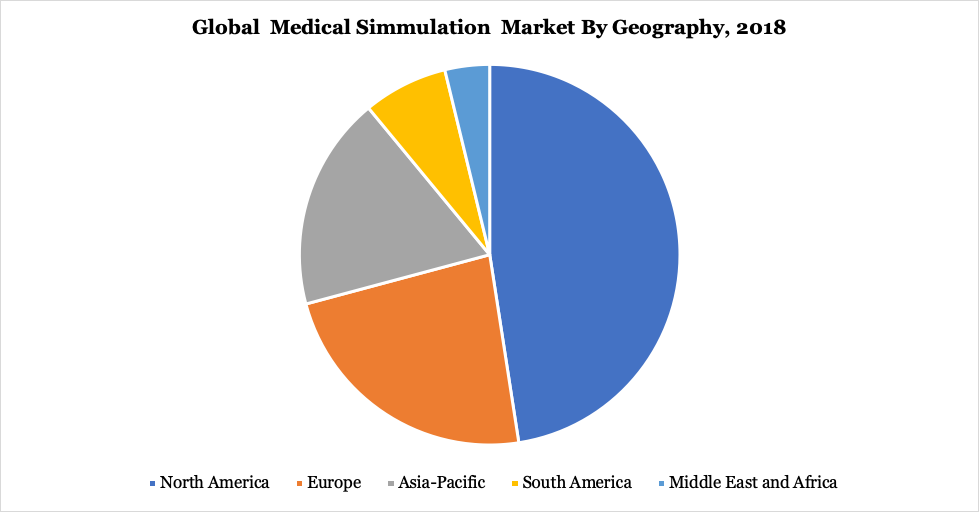
The global medical simulation market size was valued at $1,421.1 million in 2019 and is projected to reach $3,190.2 million by 2027, growing at a CAGR of 14.6% from 2020 to 2027.
The global medical simulation market is segmented (on product & service) in:
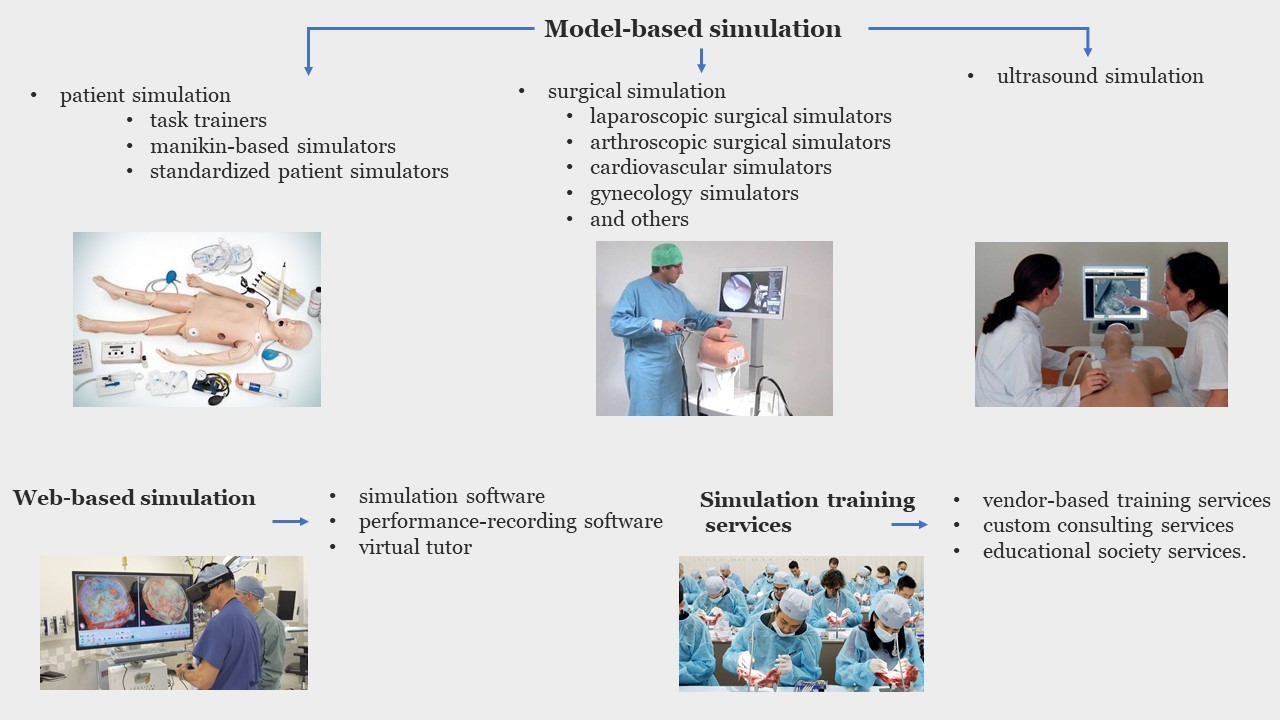
By product & service, the model-based segment generated maximum revenue in 2019, accounting for $727.47 million in 2019. The web-based simulation segment is expected to witness the highest CAGR of 15.2%. By fidelity, the low-fidelity simulators segment dominated the market in 2019 with $671.29 million. The high-fidelity segment is expected to witness the highest CAGR of 15.3% in North America, Europe, Asia-Pacific, and LAMEA. North America accounted for the largest share in the global medical simulation market. Asia-Pacific is expected to witness the highest growth rate (4).
THE COST OF TEACHING IN THE OPERATING ROOM
What is the economic cost of training a surgeon? Calhoon and colleagues addressed this question by sending cost analysis templates to program directors of 6 thoracic surgery residency programs the annual calculated cost was $483,000 per resident on average. These cost estimates for residency training do not fully account for the increased cost of OR time related to the involvement of a resident surgeon in a procedure. Cases with resident involvement (>85% of 1030 Jabbour & Snyderman cases) averaged 60% to 65% more time than cases without a trainee. It has been argued that the increased time required to train surgeons does not increase the cost for the hospital directly, but rather is primarily a “cost” to the attending surgeon, as a missed opportunity cost for performing more operative procedures during the same amount of time. However, several studies have demonstrated significant added costs related to surgical trainee involvement (2).
Other hidden costs of training surgeons in the OR include surgical complications and additional morbidity from prolonged anesthesia. A surgical complication may require additional therapy, prolong hospitalization, and incur legal costs. Surgeries that extend beyond regular work hours increase labor costs (overtime) and have an opportunity cost for the surgeon and the hospital (2).
While it is clear that healthcare simulation is key to reduce patient risk and accidental deaths, there is little information on the economic savings it brings to the Health System. Economic evaluation of simulation-based medical education will be decisive to demonstrate an improvement in trainee performance and health outcomes in order to justify investments (5).
Those are the most relevant published patents from some of the most active companies in the healthcare simulation market:
Some of the most important simulation centers in Spain are mentioned below:
HOSPITAL-BASED
| Center | Center name | Website |
 |
Centro de Simulación IDEhA | link |
 |
Vall d’Hebron Centro de Simulación Clínica Avanzada (VHiSCA) | link |
 |
Hospital virtual Valdecilla | link |
 |
SIMCLINIC. Hospital Clinic de Barcelona y UB | link |
 |
Aula de Simulación. Hospital Universitario La Paz (Madrid) | link |
 |
Área de Simulación Clínica y Seguridad del Paciente. Hospital Universitari i Politècnic La Fe – Valencia | link |
OTHER SIMULATION CENTERS
| Center | Center Name | Website |
 |
CISARC – Centro Internacional de Simulación y Alto Rendimiento Clínico | link |
 |
4DHEALTH – Innovation Simulation Center | link |
 |
CMAT – Complejo Multifuncional Avanzado de Simulación e Innovación Tecnológica | link |
 |
Centro de simulación, Facultad de Medicina, Universidad de Navarra | link |
 |
Centro de Simulación Universidad Francisco de Vitoria (Madrid) | link |
 |
Hospital simulado. Universidad Europea de Madrid | link |
 |
SATSE-CIDEFIB. Centro de Innovación y Desarrollo de Enfermería y Fisioterapia de les Illes Balears | link |
 |
Centro Usuario Unidade de Cirurxía Experimental-Centro Tecnológico de Formación. laCoruña | link |
1.-Financial barriers
The scientific community agree that the main limiting factors for the large-scale adaptation of surgical simulation in hospitals and teaching institutions are primarily due to the high cost of developing and maintaining this high-tech solution. This results from the lack of appropriate business model that motivates companies to develop surgical simulators along with the relatively small market size (1).
As we have explored, there may be an opportunity for hospital systems, malpractice insurance companies, and even health insurance companies to invest heavily in surgical simulation, because all of these entities have the potential for financial savings by increasing the technical skills of surgeons and improving communication of surgical teams. Until this occurs, departments may consider using current funds earmarked for didactic purposes and redirecting them to simulation education. Incentives could be given for faculty who convert traditional didactic activities to simulation-based interactive sessions. Industry may be another avenue of support. Already, there is a significant industry support for healthcare education, for the development of simulation laboratories, “in-kind” donation of industry products for simulation, and industry-supported educational opportunities. But educators and residents must be conscious of and properly disclose these industry relationships. As proposed by the scientific community, increasing funding from philanthropic sources or grant funding may minimize such reliance on industry support (2).
2.-Technical barriers
Another main barrier in simulation training is that most solutions are still not realistic enough, thus making irreplaceble the direct practice with patients. Moreover, in order to be financially successful, the simulator must be capable of offering the following features: (a) multifunctional training for many different specialities, (b) have the ability to train different levels of expertise, and (c) must be integrated into several aspects of the medical practice such as preoperative planning, research and virtual prototyping of instruments or equipment (1).
3.- Lack of standards in assessment metrics
Assessment methods and the metrics used should be standardised since there are still no uniform tests or reporting schemes available, which makes it difficult to determine the correspondence between different training approaches (1).
4.- COVID-19 pandemy
COVID-19 has an unprecedented impact on medical education worldwide, leading to cancellation of lectures, exams, clinical rotations, and ultimately temporary closure of medical schools.
In March 2020, the International Nursing Association of Clinical Simulation and Learning (INACSL) and the Society for Simulation in Healthcare (SSH) issued a statement on the ‘use of virtual simulation as a replacement for clinical hours’ during the pandemic caused by COVID-19. The use of virtual simulation technologies is likely to be adopted during the pandemic to enhance and strengthen procedural and patient care skills. Further, increase in use of remote learning with the help of screen-based simulation, augmented reality/AR, mixed reality, blended and/or extended reality, and virtual reality/VR is expected to drive growth of the virtual medical simulation market (4).

Touch Surgery - Secure storage for your surgical videos and data
Touch Surgery™ Enterprise (From Methronic) is our cloud solution for surgical videos, designed for you to securely access and share your videos. Our AI-powered DS1 computer records, anonymizes and uploads your videos automatically, straight from the OR.
https://www.touchsurgery.com/ // https://www.youtube.com/channel/UCAU6QOyPVd3AIQvUinHgXhQ
LEVELEX - Video Games for doctors
Level Ex creates video games for doctors that capture the challenges of practicing medicine. We’ve carved out a distinct space at the intersection of medicine and entertainment, bridging gaps in the healthcare industry through state-of-the-art video game technology and design.
https://www.levelex.com/ // https://www.youtube.com/channel/UCA6CXfLvPRra93Zdzvjb2zg
VIRTA Med - mobile surgical simulation lab
Medical education has come into the spotlight as many surgeons have had reduced time in the operating room due to COVID-19 precautions. As a global leader in medical simulation training, Swiss-based VirtaMed will use the coming months as a unique opportunity to provide courses with their latest surgical simulators in hospitals. From St. Gallen to Geneva, surgical departments will welcome a mobile simulation lab that is kitted out with virtual reality simulators and run by an expert team.
https://www.virtamed.com/en/news/switzerlands-first-mobile-surgical-simulation-lab/- ElHelw, M. A. (2020). Overview of Surgical Simulation. arXiv preprint arXiv:2005.03011.
- Jabbour, N., & Snyderman, C. H. (2017). The economics of surgical simulation. Otolaryngologic Clinics of North America, 50(5), 1029-1036.
- Anton, N. E., Gardner, A. K., & Stefanidis, D. (2020). Priorities in surgical simulation research: What do the experts say?. The American Journal of Surgery, 220(1), 95-99.
- https://www.alliedmarketresearch.com/medical-simulation-market
- Lin, Y., Cheng, A., Hecker, K., Grant, V., & Currie, G. R. (2018). Implementing economic evaluation in simulation‐based medical education: challenges and opportunities. Medical Education, 52(2), 150-160.
- Helder, M. R., Rowse, P. G., Ruparel, R. K., Li, Z., Farley, D. R., Joyce, L. D., & Stulak, J. M. (2016). Basic cardiac surgery skills on sale for $22.50: an aortic anastomosis simulation curriculum. The Annals of thoracic surgery, 101(1), 316-322.
Edu Soler
Science, healthcare and business are the three pillars that drive me nowadays. I love to engage new people in the adventure of healthcare innovation and always keep on learning from them. I am highly motivated with my participation in performing teams worldwide.
All stories by: Edu Soler







Leave a Reply